The History of TMS: What it is, How it Works, and Its Effectiveness for Treating Depression
The History of TMS: What it is, How it Works, and Its Effectiveness for Treating Depression
MAY 2
—
Studies have shown that transcranial magnetic stimulation (TMS) can be 3x more effective for treating depression when compared with traditional approaches. This breakthrough has sparked calls for continued research into the technology, with early signs suggesting that the treatment method could prove highly effective across several fields of psychiatry.
But what is TMS and how does it really work? This article will explore the 190 years of rich scientific history that produced a ground-breaking mental health treatment protocol for modern-day patients
An introduction to TMS: One of the most effective treatments for mental health disorders in the 21st century
According to The American Journal of Preventive Medicine, more than 1-in-10 Americans reported a significant bout of depression in the past 12 months. However, traditional treatments for depression have limited effectiveness, with SSRI medications such as Prozac achieving remission in only 27% of cases.
The worrying rise of mental health disorders over recent decades has rightly sparked calls for greater awareness and more effective treatments. And, with the emergence of TMS, there is renewed confidence among world-leading medical researchers that we now have the technology to treat major depressive disorder (MDD) in almost 80% of patients.
What is TMS?
Transcranial Magnetic Stimulation (TMS) is a non-invasive brain stimulation technique. It works by using electromagnetic coils to generate brief, powerful pulses that can target specific regions of the brain. These pulses activate or inhibit neural pathways, helping to improve neural communication and alleviate symptoms that are associated with various mental health conditions.
What are the applications of TMS in mental health treatment?
The FDA has approved TMS for the treatment of Major Depressive Disorder (MDD). It is most commonly used in cases where traditional antidepressant medications have been ineffective or poorly tolerated.
Research has also shown promising results in using TMS to reduce the severity of Obsessive-Compulsive Disorder (OCD) symptoms, and that it may help alleviate symptoms of anxiety for patients suffering from Post-Traumatic Stress Disorder (PTSD).
How is TMS different from other mental health treatments?
Traditional psychopharmacological treatments, including both medication and talk therapy, may not suit all patients. TMS provides an alternative that can be used in conjunction with other treatments, helping to unlock a more comprehensive approach to mental health care that is effective, safe, and personalized.
The Origins of Transcranial Magnetic Stimulation (TMS)
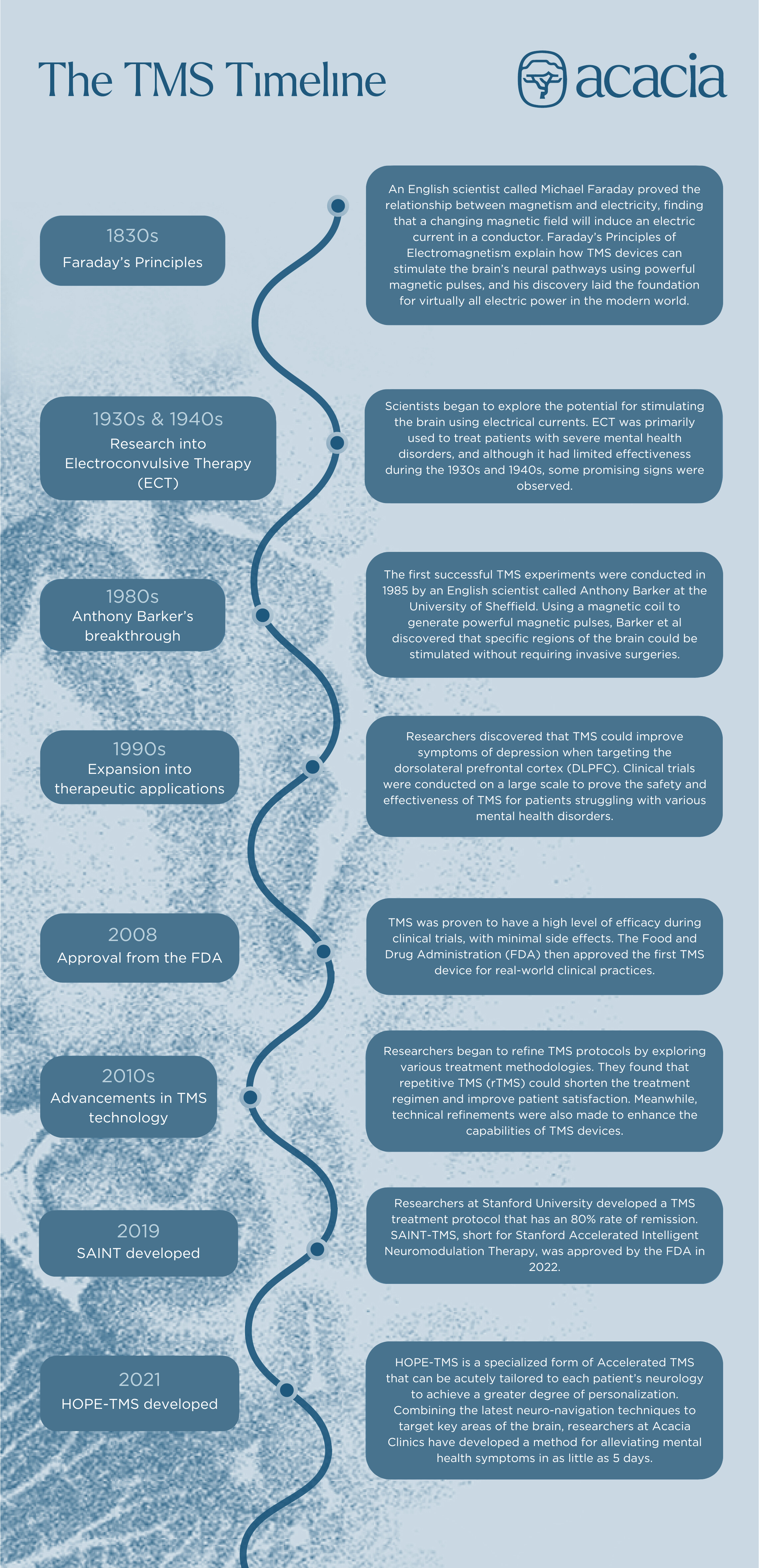
The origins of TMS can be traced back to the late 19th century and early 20th century, when scientists began exploring the idea of using electromagnetic induction to stimulate the brain’s neural pathways.
Breakthrough discoveries from key figures such as Michael Faraday and Anthony Barker encouraged scientific researchers to explore the efficacy of electromagnetism for a variety of therapeutic applications, which laid the foundation for TMS as we know it today.
Early experiments with electromagnetism
In the 1830s, an English scientist called Michael Faraday laid the groundwork for the development of TMS through his pioneering work on electromagnetism. Faraday’s principles of electromagnetic induction describe how a changing magnetic field can induce an electric current in a nearby conductor.
Specifically, Faraday demonstrated that when a magnetic field intersects a conductor, it creates an electric current in that conductor. This principle is the basis for the operation of electric motors, generators, and transformers, and it also underpins the functioning of TMS devices.
Faraday’s principles encouraged scientific research into brain stimulation, where electrical currents are applied directly to the brain to induce seizures. Experiments in electrotherapy and electroconvulsive therapy (ECT) were conducted in the 1930s and 1940s, exploring the efficacy of electromagnetism as a treatment for severe mental disorders like schizophrenia and depression.
While ECT was effective in some cases, the treatment was associated with significant side effects such as memory loss and cognitive impairment. It was clear that there was still work to be done.
Anthony Barker’s breakthrough
Building upon Faraday’s principles and early ECT experiments, researchers began exploring the possibility of producing electrical currents in the brain without direct electrical stimulation. The intention was to prove that the brain could be stimulated without subjecting the patient to the same discomforts that had marred ECT research.
In 1985, a team led by Anthony Barker at the University of Sheffield conducted the first successful TMS experiments on the human brain. They used a powerful magnetic coil to generate brief magnetic pulses that could penetrate the skull non-invasively, stimulating specific brain regions without causing physical damage.
These early experiments demonstrated that TMS could safely activate specific cortical regions, such as the motor cortex, leading to observable muscle twitches. The effect of powerful magnetic bursts as a method for stimulating the brain paved the way for further research into the therapeutic applications of TMS in various neurological and psychiatric disorders.
Expansion into therapeutic applications
By 1993, researchers had observed the antidepressant effects of TMS and began investing the potential use of TMS for treating depression. One of the pioneering studies was conducted by Mark George and his team at the University of South Carolina, which showed promising results for sustained TMS treatment over multiple weeks in improving depression symptoms.
These early studies laid the groundwork for larger clinical trials, evaluating the efficacy and safety of TMS while considering variables such as treatment frequency. Due to a growing body of evidence that supported TMS as a highly effective treatment with few side effects, the United States Food and Drug Administration (FDA) approved the first TMS device for the treatment of major depressive disorder in 2008.
FDA Approval, Widespread Adoption, and Continued Advancements in TMS Technology
The FDA’s approval of the technology marked an inflection point in TMS research and development. The refinement of TMS protocols was encouraged, and the widespread adoption of TMS in specialized clinical practices provided real-world evidence to support patient satisfaction claims.
Repetitive transcranial magnetic stimulation (repetitive TMS) was explored as a means for refining the efficiency of TMS without sacrificing its effectiveness. Researchers found that repetitive TMS produced remission in 64% of patients — far outperforming alternative treatments such as SSRI medication.
Following continued research from Stanford University, further refinements were made. The development of Stanford Accelerated Intelligent Neuromodulation Therapy (SAINT) marked another major milestone in the history of TMS, as several studies found that SAINT produced an 80% rate of remission for patients with mood disorders.
In addition to advancements in treatment protocols, coil design has also continued to evolve. Researchers have developed various coil designs to optimize the focality, depth, and efficiency of the magnetic field delivery, such as those used in devices developed by Magnus Medical specifically for the delivery of SAINT-TMS, which were approved by the FDA in 2022.
The Future of TMS
While TMS has come a long way from Barker’s first experiments on the human brain, it remains a hotbed of psychiatric research to this day. Leading scientists continue to explore transcranial magnetic stimulation for emerging applications such as smoking cessation and chronic pain relief, and there are sustained efforts to refine TMS treatment approaches further.
Here are some of the main areas of development that could help shape the future of the technology.
Advancements in personalized treatment protocols
TMS solves key drawbacks with traditional depression treatments, enabling clinicians to provide fully personalized treatment protocols that can supplement existing methods. This multimodal approach combines TMS with other modalities such as cognitive behavioral therapy and medication, representing a new frontier for researchers as they explore the most effective ways to improve symptoms of depression.
Additionally, researchers continue to explore the efficacy of TMS when integrated with neuroimaging techniques. Functional magnetic resonance imaging (fMRI) and diffusion tensor imaging (DTI) allow for precise targeting of specific neural networks based on each individual’s brain anatomy. For patients, this unlocks new ways to personalize TMS treatment protocols according to their specific needs.
Smoking cessation
Beyond its established use in treating depression and other psychiatric disorders, researchers are exploring TMS as a treatment for smoking cessation. Several studies have investigated the use of TMS as a potential aid for smoking cessation by modulating brain regions associated with addiction and craving.
Researchers have targeted areas such as the dorsolateral prefrontal cortex (DLPFC) and the insula, which are respectively involved in cognitive control and the processing of smoking-related cues. Initial studies have shown promising results, with TMS reducing cravings and improving abstinence rates when combined with behavioral therapies.
Chronic pain
TMS has shown potential in managing various types of chronic pain, including neuropathic pain, fibromyalgia, and migraines. By targeting the primary motor cortex or dorsolateral prefrontal cortex (depending on the type of pain being treated), several studies have reported significant pain reduction and improved quality of life in patients undergoing TMS treatment for chronic pain conditions.
Neurodegenerative disorders
TMS is being investigated as a potential therapeutic approach for neurodegenerative disorders such as Alzheimer’s, Parkinson’s, and multiple sclerosis. Researchers are exploring whether modulating brain activity can slow the progression of these diseases and improve motor functions.
The bottom line: 190 years of scientific research (and counting) for the future of mental health care
This was a brief summary of the remarkable journey taken by TMS over the course of its history. Traditional depression treatments are often associated with significant side effects and limited effectiveness, yet TMS has emerged as a safe and effective alternative that can help people overcome years of suffering when it comes to depression, anxiety, mood disorders, and other mental illnesses.
HOPE-TMS, an accelerated TMS protocol developed by Acacia Clinics, provides a personalized, efficient, and effective method for alleviating symptoms of mood disorders. HOPE was developed by scientists on the cutting edge of psychiatry to combine the most advanced TMS treatment protocols, helping patients overcome symptoms with a 77% response rate in 5 days of treatment.
We encourage anyone who may be suffering from a mental health condition to reach out to us for more information about the treatment options available.